
Sustainable Construction
Lorem ipsum dolor...
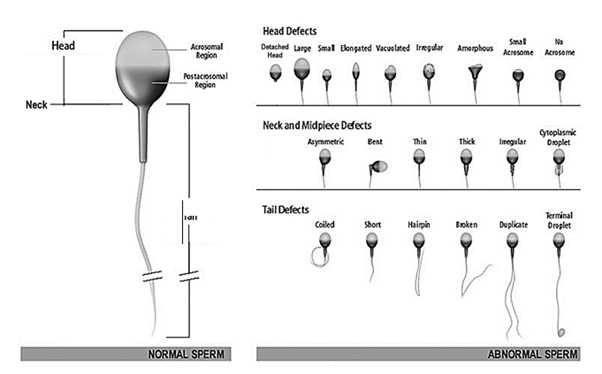
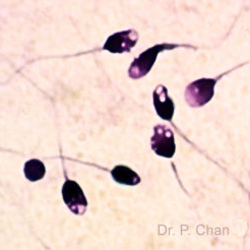
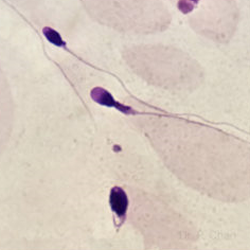
The value of human sperm morphology assessment is not only the limited prognostic value regarding spontaneous pregnancies or outcome of ART, but even more the diagnostic information about the functional state of the male reproductive organs, primarily the testicles and epididymides. For the evaluation of the male reproductive organs, it is not sufficient to only determine the proportion of “normal” spermatozoa. It is important to evaluate the specific morphology of head, neck/midpiece and tail, and the possible presence of abnormal cytoplasmic residues.
All human ejaculates contain spermatozoa with a wide range of different morphological appearances. Earlier definitions of sperm morphology were based primarily on experiences from veterinary medicine and microscope investigations.
The criteria presented here were developed from investigations of the morphology of spermatozoa able to penetrate cervical mucus and bind to the zona pellucida.
The term “normal” spermatozoon is in some ways ambiguous, causing misunderstandings and even academic conflicts. One general meaning of “normal” is a quality that is common in, for instance, a population. This is not true for “normal sperm morphology” in humans. Another meaning is that it indicates that the cell or individual is not affected by disease, but a normal morphology does not mean that the sperm cannot carry another cause of pathology (e.g. immotile tail or damaged DNA).
The variable morphology of human spermatozoa makes assessment difficult, but observations on spermatozoa recovered from the female reproductive tract, especially in postcoital endocervical mucus and also from the surface of the zona pellucida, have helped to define the appearance of potentially fertilizing (morphologically normal or, better, “ideal” or “typical”) spermatozoa. By the strict application of certain criteria of sperm morphology, relationships between the percentage of “normal” forms and various fertility end-points (time to pregnancy, pregnancy rates in vivo and in vitro) have been established, which may be useful for the prognosis of fertility.
The World Health Organization also published their own sperm analysis criteria. As of 2021, they consider the presence of 4 percent and higher of sperm having normal morphology as the ideal sample composition for fertility.

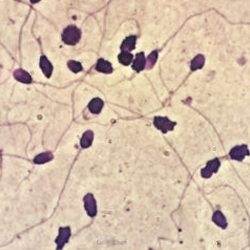
Normal-shaped sperm
Macrocephaly sperm
Microcephaly, or small-head sperm

Pinhead sperm
Tapered head sperm
Thin head sperm
Decondensing head sperm
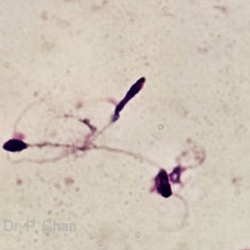
Headless sperm
Tail-less sperm
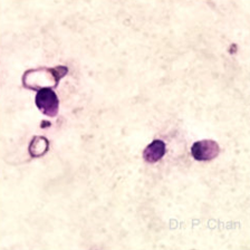
Nuclear vacuoles sperm

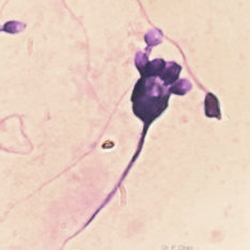
Multi-head sperm
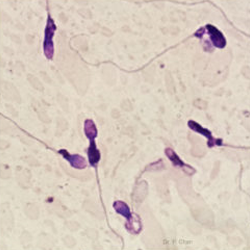
Thick, swollen neck
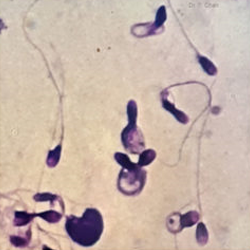
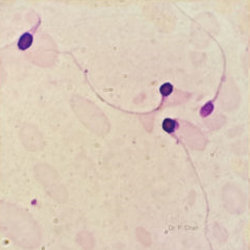
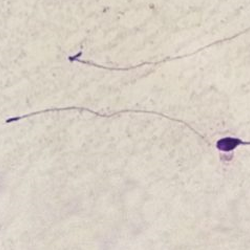
Coiled-tail sperm

Stump tail sperm